Learning Outline
Lymphatic System & Immunity
A&P 2
Lymphatic System
General structure and function
Part of “circulatory system”
- Lymph (lymphatic fluid)
- Lymphatic vessels
- Lymph nodes and lymph nodules
- Tonsils
- Thymus
- Spleen
- Fluid balance
|
- Returns water, proteins, etc. from tissues back to blood
- Immunity
- Transports lipids from the digestive tract
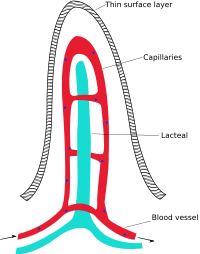
- Lacteals (lymph capillaries) in intestine transport fatty lymph called chyle
Starling’s Law of the Capillaries
In a capillary, there are inwardly directed forces and outwardly directed forces that are balanced or imbalanced
- Osmotic pressure
- Hydrostatic pressure (pressure of fluid against a membrane)
At the arterial end of a capillary
- Outwardly directed forces (mostly blood pressure) causes net diffusion of water and small solutes OUT of the blood (and into the IF [interstitial fluid])
At the venous end of a capillary
- Inwardly directed forces (mostly tissue fluid pressure and osmotic pressure of the blood plasma) causes net diffusion of water and small solutes INTO the blood (and out of the IF)
About 10% (varies greatly) of the fluid that OUGHT to return to the blood capillary does not
- This “extra” interstitial fluid (IF) in the tissue may accumulate, causing painful swelling and potentially fatal damage to the tissue
- Blood would also loose too much fluid to maintain health
- The lymphatic system includes a system of vessels that drains this excess fluid away and returns it to the blood supply
Lymphatic drainage
- Blind-end tubules that begin in a tissue and continue as tributaries to larger and larger vessels, like creeks running into large streams, into rivers, into the lake
- Lumen (hollow part) of capillaries is “always open” like storm drainage pipe because tiny fibers attached to surrounding tissue cells hold it open from the outside
- This allows water and small particles to drain into the capillaries easily (without much of a pressure gradient)
- The drained fluid is now called “lymph” or “lymphatic fluid”
- Numerous SL (semilunar) valves keep lymph from flowing back toward tissue
- Drain away excess fluid as described above
- Also drain away fats absorbed in the digestive tract (otherwise the fats would increase blood viscosity and slow blood flow during absorption of a meal)
General plan of lymphatic drainage (above)
Intestinal villus
- Lymphatic vessels eventually all drain into the . . .
- Right lymphatic duct
- Drains lymph from the superior right quadrant of body —-into the right subclavian vein (just before the systemic blood enters the right atrium of the heart)
- Thoracic duct
- Drains lymph from the lower right quadrant and entire left side of body into the left subclavian vein
- Right lymphatic duct
- Numerous SL valves and lymph nodes (and other lymphoid organs)
Lymphokinesis (kinesis = “movement”)
- One-way flow (linear; unlike “circular flow” of cardiovascular system) toward the blood/heart
- Lymphatic pump
- Similar to venous pumps
- Lymphokinesis averages about 125 ml/hr (that’s 3 L/day)
|
Elephantiasis Also known as lymphatic filariasis, this condition occurs when parasitic worms (any of several types of filaria worms) infest the lymphatic system. The filaria are transmitted by mosquitoes to the blood and can build a population in the lymph nodes, blocking fluid drainage from arms, legs, genitals, or breasts. It is called elephantiasis (literally, “elephant condition”) because in extreme cases, the arms and legs look like the limbs of an elephant. Elephantiasis affects over a 100 million people around the world. However, most cases are not as extreme as in these photos. |
|
Lymphatic drainage of the breasts — a special case
- Superficial lymphatics
- Deep lymphatics
- Lymphatic anastomoses
- Superficial with deep
- Across median
- With abdominal lymphatics
- With pectoral muscles
Important in infections (mastitis) and cancer (breast cancer) because bacteria or cancer cells can easily migrate to other parts of the body, making things even more serious
Lymphoid organs
Lymphoid organs have flow-through of lymph (and/or blood)
Lymphoid organs have lymphoid tissue, which is made up of developing WBCs
Lymph nodes
- Each is a tiny (1-20+ mm) fibrous capsule divided into many chambers
- Each chamber or “sinus” has may fine (reticular) fibers suspending a lymph nodule made up of lymphoid tissue
- Lymphoid tissue is packed WBCs
- Germinal center is the the interior portion of a nodule
- Where B-lymphocytes begin the last stages of development (then are released from outer part of nodule)
- Lymph enters node through afferent lymphatic vessels and leaves the node through efferent lymphatic vessels
- Filtration in lymph nodes
- As lymph flows through lymph node, lymph is mechanically filtered by fibers (large chunks get stuck)

- Lymph is biologically filtered when phagocytes (reticuloendothelial cells) consume the particles or otherwise attack the particles
- Sentinel lymph node (SLN) — first lymph node to which a cancerous tumor can spread (clinically important)
- As lymph flows through lymph node, lymph is mechanically filtered by fibers (large chunks get stuck)
Tonsils
- Several sets of lymph nodules in throat
- Lingual tonsils – base of tongue
- Pharyngeal tonsils – posterior wall of nasopharynx (above soft palate)
- Called adenoids if they become enlarged, possibly blocking breathing
- Palatine tonsils
- Oval thickening of mucosa on each side of oropharynx
- Most prominent of all tonsils; have 10-20 crypts(pits)
- Tubal tonsils
- In pharynx, near openings of auditory tubes (Eustachian tubes)
Peyer patches
- Now more often called aggregated lymphoid nodules
- Located in the instestinal wall
Thymus
- Also an endocrine gland, found in chest in front of or slightly above the heart (mediastinum)
- Largest at puberty, then shrinks slowly over time (almost gone in advanced old age [even older than Kevin])
- Cortex — lymphoid tissue
- Site of T-lymphocyte (T-cell) development (lymphocytes become T-cells under the influence of thymosin hormones)
- Medulla — thymic corpuscles (function not clear; may be be where older cells are broken down)
- Located in left upper part of abdomen, under diaphragm and tucked behind the stomach (left hypochondrium)
- Like a giant lymph node for blood
- Ovoid organ with fibrous outer capsule
- Many sinuses that contain lymphoid tissue (incl. reticuloendothelial cells) for the filtering of blood (including RBC/platelet destruction)
- White pulp
- Dense masses of whitish lymphoid tissue in core of each sinus
- Red pulp
- At outer part of each sinus, made up of blood-filled reticular tissue
- Includes cords of white blood cells
- White pulp
- Hematopoiesis
- RBCs (before birth)
- Nongranular leukocytes
- Blood reservoir
- Tissue repair
- Mobilizes monocytes (from red pulp) during tissue injury
- Removes and repairs damaged tissue
- Mobilizes monocytes (from red pulp) during tissue injury
Immunity
Hint — Review types of pathogens in “Mechanisms of Disease” at end of Chapter 1 of textbook: bacteria, viruses, protozoa, fungi, worms, etc.
The body’s defense
Immunity is protection/defense ![]()
Immunity is carried out by many cells and tissues of the body, not just those classically identified as “immune cells” or “immune tissues”
Defense / protection against variety of “enemies”
- Nonself particles have unique identifying marker molecules
- Similar to the insignia of enemy aircraft, vehicles, soldiers
- Self-tolerance—we do not attack our own cells
- Examples of “enemies”
- Pathogens (see above)
- Cancer cells (your own cells that have become cancerous)
- Physical damage (burns, cuts, etc.)
- Innate immunity
- Called “innate” immunity because it does not require prior exposure to a pathogen
- Also called nonspecific immunity
- Mechanisms that are “on standby” at all times and are effective against a variety of different “enemies”
- Innate immune mechanisms respond rapidly (always “on alert”)
- Adaptive immunity
- Called “adaptive immunity” or “acquired immunity” because it changes to work against new pathogens upon exposure to them
- Also called specific immunity
- Mechanisms that are effective against specific (one kind only) “enemies”
- Adaptive immune mechanisms respond more slowly because they take time to prepare and develop
Note — Immunology is a complex and rapidly changing discipline. We will be looking at a simple overview of immunology to prepare you for further work in this area later in your studies.
Innate (nonspecific) defenses
There are many innate strategies; here we discuss just a few of them
- Many of these innate defenses also work in cooperation with, or are supplemented by, additional adaptive defense mechanisms
Species resistance
Lines of defense (as in military model)
Surface barriers – skin and mucous membranes
Phagocytes – neutrophils, eosinophils, macrophages
- Antigen-presenting cells (APCs) digest the enemy particle and display the unique protein markers to signal the adaptive immune system
- Examples
- Macrophages — large, phagocytic cells found in many areas of the body
- Dendritic cells (DCs) — branched phagocytes, often at/near external barriers
Natural killer (NK) cells
- NK cells are lymphocytes that “patrol” the body, looking for abnormal cells (esp. cancer cells and virus-infected cells) to kill
- NK cells kill by direct contact with enemy cell
- NK cells each have two receptors
- Killer-activating receptor binds to common cell markers (thus, binds even to self cells)
- Killer-inhibiting receptor binds to certain self markers, thus preventing killing of self cells
- The self markers are MHC (major histocompatibility complex) proteins unique to every individual
- Kill by various methods
- May release perforins, which are proteins that form holes in the plasma membrane of the cell to be killed
- Sodium diffuses in, then water osmoses inward, causing the cell to swell and burst (cytolysis)
- In nucleated cells, this influx of ions may trigger apoptosis (programmed cell death), also resulting in cytolysis
- May also release granzymes that can enter the cell and trigger apoptosis
- May release perforins, which are proteins that form holes in the plasma membrane of the cell to be killed
- NK cells each have two receptors
Defensive proteins (cytokines)
- Interferons (IFNs) are released by dying, virus-infected lymphocyte or other cell

- Interferons “call in” other immune cells (NK cells and macrophages) that destroy virus-infected cells, protecting the body from further spread of viral infection
- Interferons also “interfere” with the ability of viruses to replicate in other nearby cells —also stopping the viral infection
- Interferons are paracrine agents, regulating nearby cells
- Complement is a group of about 20 different plasma proteins
- Individual complement proteins are designated C1, C2, C3, and so on
- Complement molecules are activated in a cascade of chemical reactions triggered by innate or adaptive mechanisms
- Complement can act directly, as do perforins
- Form MACs (membrane attack complexes) that poke holes in the outer membrane
- Complement can act indirectly as a chemotactic agent or regulating immune cells in some other way
- Chemotaxis

- Chemical attractants are released from damaged tissue cells and immune system cells to “call over” immune cells to the site of injury
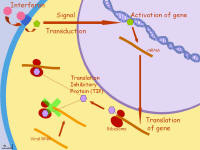 |
Interferon activity in a virus-infected cell. Click the image to enlarge it Click here for the animated version (PowerPoint slide) |
Inflammation and fever
- Inflammation (the inflammatory response)
- Set of reactions in response to injury
- Four principle signs of inflammation
- Redness (flush)
- Warmth (heat)
- Pain
- Swelling (edema)
- Inflammation mediators are chemicals that regulate the inflammatory response
- Four principle signs of inflammation
- Set of reactions in response to injury
HINT — The inflammatory response is summarized in textbook Figure 21-3
- Fever
-
- Pyrogens (literally “fire makers”)
- Chemical factors released by pathogens or immune cells
- Mild, moderate fever increases body temp slightly
- Increases efficiency of immune mechanisms
- Decreases efficiency of pathogen function
- High or prolonged fever
- Can denature (change shape of) proteins, thus disrupting enzyme activity bodywide —perhaps leading to death
Toll-like receptors (TLRs)
- Pattern-recognition receptors (PRRs) in the membrane of “self” cells
- Are triggered by various “nonself” marker patterns (such as viral RNA)
- When triggered, can stimulate various innate responses
- Named for the gene that makes them (similar to the Toll [“weird”] gene)
Adaptive (specific) defenses
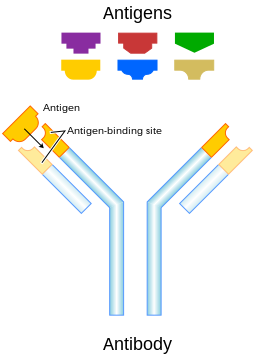
Two strategies of adaptive defense ![]()
- Antibody-mediated immunity
- Uses antibodies (immunoglobulins [Ig])
- Also called humoral immunity because antibodies are dispersed in the blood plasma (humor = “body fluid”)
- Antibodies are Y-shaped plasma proteins made by B-lymphocytes (B cells) that bind to specific antigens (markers or particles that have a complementary shape to the active site on an antibody molecule) and cause them harm
- The “B” in B cell refers to “bursa-equivalent tissue,” where B cells develop
- In humans, B tissue is found in the yolk sac and fetal liver, then later the red marrow
- B cells eventually migrate to lymphoid tissue (nodes, nodules) to complete their maturation
- Antibody-mediated immunity is like “shelling” the “enemy” —the antibodies are like “homing missiles” directed as specific distant targets
- Cell-mediated immunity
- Uses cells (T-lymphocytes = T cells)
- The “T” in T cell refers to the thymus, where T cells develop
- Also called cellular immunity
- T cells directly attack another cell such as an infected cell or cancer cell
- Uses cells (T-lymphocytes = T cells)
Specialized lymphocytes carry out adaptive immunity
- Thus, lymphocytes are the “soldiers” of adaptive immunity
- Lymphocytes are often identified by their CD (cluster differentiation) markers
- CD4 or CD8, for example
- Triggering adaptive responses requires BOTH of two signals

- Stimulate antigen receptor
- Antigens are markers that identify nonself particles
- For example, antigens presented by APCs (see above)
- B cells can also detect free-floating antigens in the plasma
- Prior to recognizing an antigen, lymphocytes are known a naïve cells, or virgin cells, or inactive cells
- Stimulate cytokine receptor
- Cytokines are regulating chemicals
- Stimulate antigen receptor
Effector and memory cells
- Effector cells are the cells that actively participate in “the battle” against “the enemy”
- Effector cells usually die during or just after the “battle”
- Memory cells are inactive copies of the effector cells that are held as “reserves” in case the same enemy attacks later
- Memory T cells and memory B cells can quickly be activated or “called up to the front” and become effector cells if the same enemy attacks again at a later time
Sounding the alarm
- Macrophages, DCs, or other APCs (antigen-presenting cells) ingest the “enemy” and incorporate the enemy markers on the surface of the APC
- This display of “enemy antigens” then triggers a helper T cell (= T4 cell = CD4 cell) with complementary receptors by releasing interleukin 1
- Interleukin 1 activates the helper T cell, which divides into many identical daughter cells (the group of identical cells is called a clone)
- Some of the cells remain inactive “reservists” as memory helper T cells
- Some of the cells become effector cells, releasing interleukin 2, which activates an appropriate (one with the proper receptors) T cell or B cell
- Recall that cytokine is the general name for any chemical signal in sent from immune cells (e.g. interleukins [ILs])
Mobilizing the troops
- The activated T cell or B cell then divides into memory T or B cells (“reservists” that may be “called up to the front” later) and effector T or B cells that now “attack” the “enemy”
Attacking the enemy
- Antibody-mediated immune response (the strategy of B cells)
- Activated B effector cells are usually called plasma cells
- Plasma cells secrete antibodies into the plasma
- Antibodies bind to complementary antigens that are free or on surface of “enemy” cell (can’t get inside cells, however)
- Examples of antibody actions
- Neutralization — bind to receptors on the surface of a virus, thus rendering the virus incapable of infecting cells, and this also marks the virus for destruction by other immune cells
- Agglutination — as antibodies bind to several different “enemies” at once, they clump together and can be gobbled by phagocytes
- Activation of complement — complement “blows up” the “enemy cell”
- Classes of antibodies (M, G, A, E, D)
- IgG (immunoglobulin G) is most abundant in the blood (75% of plasma Ig)
- Activated B effector cells are usually called plasma cells
- Cell-mediated immunity
- Activated T effector cells are called cytotoxic T cells (literally “cell poison” T cells)
- Also called cytolytic cells, T8 cells, or CD8 cells
- Activation requires BOTH
- Cytotoxic T cells must recognize combined self-nonself marker on an antigen-presenting cell
- Interleukin 2 from a helper T cell
- Cytotoxic T cells “grabs” or “touches” enemy and releases perforins, which “blows up” the enemy
- Activated T effector cells are called cytotoxic T cells (literally “cell poison” T cells)
 |
Immune defense
Click this image for an enlarged view of a “plan of attack” using both antibody-mediated immunity and cell-mediated immunity |
Retreats and future battles
- Sounding “retreat” — turning off the immune response
- As antigen levels decline and thus the “battle is being won” suppressor T cells release chemicals that cause B and T cell “troops” to “stand down” or stop attacking
- The first encounter with an enemy is called the primary response
- Successful first encounters cause memory cells to be made and held in reserve for possible future encounters
- Secondary responses occur when memory cells are activated during subsequent encounters with a previous enemy
- Secondary encounters are strong and swift —quickly defeating the enemy
FYI: Click here for a detailed poster of the development of various immune cells. This poster shows how intricate the process really is!
- Active and passive
- Active immunity — when the agents of immunity are made by your own system (you have your own army)
- Passive immunity — when the agents of immunity are not made by your own system
- For example, as when you get antibodies from your mother’s milk or from an injection of serum that contains antibodies (you are using hired soldiers from another country)
- Natural and artificial
- Natural immunity — occurs “accidentally” as nature takes its course
- Artificial immunity — purposeful manipulation of immune functions for therapeutic or preventive reasons, such as vaccination
- Autoimmunity — abnormal response of the immune system in which “self” cells are attacked as if they were enemies
- Allergy (hyperimmunity) — abnormal response to an antigen (called an allergen) that is ordinarily not harmful (or overreaction to an antigen that is harmful)
This is a Learning Outline page.
Did you notice the EXTRA menu bar at the top of each Learning Outline page with extra helps?
Last updated: October 22, 2019 at 14:11 pm