Learning Outline
Digestive System & Nutrition
A&P 2
Overview of digestive anatomy and physiology
Main functions
Digestion — breaking complex (large) nutrients down into simple (small) nutrients
- Mechanical digestion — large particles into small, without changing molecular structures
- Examples — chewing, peristalsis, segmentation, mixing/churning
- Examples — chewing, peristalsis, segmentation, mixing/churning
- Chemical digestion — large molecules into small
- Examples — enzymatic breakdown of polysaccharides into disaccharides and then into monosaccharides
Absorption — moving simple nutrients from lumen (external environment) to blood (internal environment)
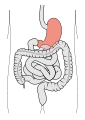
Alimentary canal
One-way digestive tract through the body ![]()
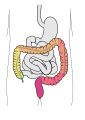
Section including the stomach and intestines is also called the gastrointestinal (GI) tract ![]()
- Each section of the canal is considered to be a primary organ
Any digestive organ that is NOT a section of the tract (for example, salivary glands, liver, pancreas) is considered to be a secondary or accessory organ of the digestive system
Hollow area, called the lumen, is functionally an extension of the external environment (contents of the lumen is not really “a part of you”)
Wall of digestive tract
Tract has four layers (coats) around the lumen
Mucosa (mucous coat) – mucous epithelium
- In many sections, this lining of the tract is folded with bumps that have bumps (fractal-like surface)
- Fractal surfaces have bumps that have bumps that have bumps —seemingly infinitely— that greatly increase surface area
- Increases efficiency of secretion of digestive juices and of absorption and at the same time allows each section to expand (like a folded cloth balloon) to accommodate more food
- Mucus (water and glycoproteins and other nifty stuff)
- Protects (from mechanical injury, stomach acid, bacterial infection)
- Lubricates (keeps food sliding along the tract)
- Aids in mixing (helps liquify and mix up ingested food)
Submucosa (under-mucous coat) – fibrous connective tissue
- Helps stabilize and strengthen mucosa layer
Muscularis (muscle coat) — smooth muscle
- Two layers — circular (inner) layer and longitudinal (outer) layer
- Stomach wall has third oblique layer under its circular layer
- Sphincters
- Thick groupings of circular muscles that acts as valves to regulate flow through the tract
- Recall that smooth muscle is involuntary muscle
- Often autorhythmic
- Basal electrical rhythm (BER) — intrinsic, rhythmic fluctuation
- Pacemaker activity similar to cardiac muscle, allowing the BER to spread to other nearby muscle fibers
- Migrating motor complex (MMC) during fasting “cleans out” the tract
- Starling’s Law of the Gut — smooth muscle contracts when stretched
- Activity of muscles is called motility
- Defecation is motility that results in movement of the feces out of the body (called “bowel movement” or BM)
Serosa (serous coat)
- Serous membrane (thin epithelial membrane coated with watery, lubricating serous fluid)
- Same as visceral peritoneum
- Same as visceral peritoneum
- Above the diaphragm this layer is instead simply fibrous connective tissue
Enteric Nervous System (ENS)
Among the muscles and other layers is a complex network of nerves
Called by some “the second brain” this network performs complex regulation of secretion and motility of various sections of the tract
Accessory organs of digestion
Exocrine glands that have ducts leading into the lumen of the digestive tract
Functional anatomy of the digestive system
Mouth (oral cavity)
- Lips & cheeks
- Palate (roof)
- Fauces (archway to throat) with uvula (dangling thing)
- Tongue (and floor)
- Teeth


General tooth structure



- Crown — part that is visible
- Covered with hard enamel
- Neck — where crown becomes the root
- Root — part inside jaw socket

- Covered with cementum
- Bound to jawbone by collagenous periodontal membrane (ligament) [peri = “surrounding” odont = “tooth”]
- Inner shell of tooth (under crown and inside root) is hard dentin tissue with hollow pulp cavity containing nerves and blood vessels
- Crown — part that is visible
- 32 permanent teeth
- Shape determines function

- Incisors (2 per quadrant) – cutting teeth
- Canines (1 per quadrant) – grabbing, tearing teeth
- Premolars (2 per quadrant) – sawing, tearing teeth
- Molars (3 per quadrant) – crushing, grinding teeth
- Human teeth are not very specialized for any of these functions
- Compare incisors/molars of horse, for example, which are extreme; or compare canines/premolars of a cat, which are extreme
Therefore, we are built to be “Swiss army knives” that can do anything—but not all that well
- Humans are omnivores
- Salivary glands

Function
- Ingestion — putting food into digestive tract (usually implies swallowing also)
- Mastication — chewing
- Deglutition — swallowing (through pharynx and esophagus to stomach)
- Gustation — tasting (chemical analysis of food)
- Digestion
- Mostly mechanical (see above)
- Perhaps some chemical (salivary amylase digests polysaccharides, but not much time for this)
- Nondigestive functions (for example — smiling, kissing, spitting, talking, singing, whistling, raspberries, licking, and so on)
Pharynx (throat)
Structure
- Three divisions
- Nasopharynx
- Behind nasal cavity
- Oropharynx
- Behind oral cavity
- Laryngopharynx
- Behind larynx (voicebox)
- Nasopharynx
- Extends to the esophagus
- Bolus (ball or chunk) of food from oral cavity enters middle of pharynx and moves into esophagus
Function
Esophagus
- Collapsible, muscular tube specialized for peristalsis (approx. 25 cm)
- Posterior to trachea and heart

- Passes through hiatus in diaphragm
- Lower esophageal sphincter (LES) is a ring of smooth muscle at opening of stomach to prevent backflow (esophageal reflux)
- Reflux can cause “heartburn” and lead to more serious complications
- Also sometimes called the cardial or cardiac sphincter
- There is also an upper esophageal sphincter (UES) that guards the opening of the esophagous from the pharynx
- Opens during deglutition
Function
- Deglutition
- Vomiting — emptying of stomach and beginning of small intestine via esophagus/throat/mouth
Stomach
- Just inferior to diaphragm

- Regions of stomach

- Cardial region
- Fundus
- Body
- Pylorus
- Curves of stomach
- Greater curvature (inferior)
- Lesser curvature (superior)
- Size varies greatly


- Folds (rugae) help mix/liquefy bolus to become chyme

- Very muscular (has 3, not 2, layers of muscle)
- Has gastric pits that include gastric glands
- Two sphincter valves control the openings
- Lower esophageal (cardial) sphincter controls superior opening
- Pyloric sphincter controls inferior opening
Function
- Storage of food until small intestine is ready
- This is the MAIN function of the stomach, other functions occur because you might as well do something with the food while it’s sitting there so you start what digestion you can ahead of time
- Mechanical digestion
- Liquifaction of bolus into chyme
- Propulsion — forward movement of chyme
- Retropulsion — backward movement of chyme
- Goblet cells produce mucus (part of “gastric juice“) that protects stomach lining and aids in mixing & lubrication
- Chemical digestion
- Hydrochloric acid (HCl)
- Produced by parietal cells of gastric mucosa
- CO2 + H2O —> H2CO3 —> HCO3– + H+
- CO2 + H2O —> H2CO3 —> HCO3– + H+
- Produced by parietal cells of gastric mucosa
- Hydrochloric acid (HCl)
- H-K pump (proton pump) moves H+ ions into gastric juice
- Parietal cells can quickly increase their surface area by 100x, thus rapidly increasing their output
- Parietal cells also make intrinsic factor (protects vitamin B12 and allows its absorption)
- Denatures (unfolds) proteins so enzymes have a shot at peptide bonds between amino acids
- Pepsin
- Produced by chief cells of gastric mucosa
- Secreted as pepsinogen (an inactive proenzyme that is later converted to active pepsin)
- All digestive enzymes do this, or else they’d eat the cell that made them
- Hydrolysis of long polypeptide chains into shorter peptide chains
- Hydrolysis, used by all digestive enzymes, uses water (H2O or HOH) to break apart subunits of macromolecules
- Absorption
- Almost NO absorption of water & nutrients in the stomach
- Chyme must move to small intestine for absorption
- If nutrients are already in their simplest form, they are almost immediately absorbed by the small intestine
- Rate of gastric emptying determines how fast a substance will be absorbed
- This is important for rapid rehydration, for example
- Gastric emptying can be hastened if
- The ingested material is dilute, if it is room temp or cooler, and if it is low in protein or fat
|
OH-X-X-X-X-X-X-X-X-X-H + H-OH Hydrolysis (hydro = “water” lysis = “break apart”) Hydrolysis breaks apart amino acids (or saccharides or fatty acids or glycerol) from one another by breaking the bond that holds them, then “plugging up” the two exposed ends with the two pieces of a split water (HOH) molecule so that the bond cannot re-form. Thus a long polymer can be broken down into many separate monomers. |
Small intestine
- Small diameter (2-3 cm) and long length (6 m)
- Three sections forming many loops in the abdominopelvic cavity
- Lined with circular folds (plicae circulares)
Function
- Receives chyme from the stomach in small spurts
- Continues mechanical digestion
- Most chemical digestion occurs here
- Absorption of most nutrients occurs here
- Most nutrients are absorbed through the brush border into the blood capillaries
- Lipids are absorbed instead into the lacteal so that the blood flow is not “gummed up” with fats and oils
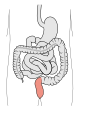
Large intestine (colon)
- Wider than small intestine (5-6 cm) but shorter (1.5-2 m)
- Muscles in wall are “bunched up” causing the large intestine to look puckered
- Pouched sections are called haustra
- Tapelike taeniae coli are longitudinal strips of muscle
- Sections
Function
- Continued digestion and absorption of nutrients
- Formation of feces
- Defecation (elimination)
- Feces tells a lot about a person’s digestive health

- Timing issues can warn of diarrhea (literally, “flow through”) or constipation
- Color, consistency can warn of health issues
- Gray feces indicates lack of bile
- Black feces indicates bleeding in early part of tract
- Red feces indicates bleeding in lower part of track
- Presence of bacteria, parasites, swallowed object
- Timing issues can warn of diarrhea (literally, “flow through”) or constipation
- Feces tells a lot about a person’s digestive health
Peritoneum
- Visceral layer (against organs)
- Parietal layer (lines abdominopelvic cavity)

- Produces lubricating peritoneal fluid
Mesenteries
- Inward folds of membrane
- Support and protect digestive glands
- Greater and lesser omentum are apronlike folds
Peritonitis
- Inflammation of peritoneum
- If infectious, can quickly spread to many organs & into blood stream
Liver
- About 1.5 kg (largest gland in the body)
- Located in right upper portion of abdominopelvic cavity -across from stomach

- Left and right lobes

- Right lobe is made up of three smaller lobes
- Lobules are microscopic subdivisions of lobes
- Each lobule processes blood and produces bile
- Sinusoids (for blood flow)

- Bile ducts collect bile as it forms
- Hepatic ducts drain bile from liver
- Common hepatic duct formed by joining of left & right hepatic duct
- Common bile duct formed by joining of common hepatic duct with cystic duct, then later the pancreatic duct
- Enters duodenum at major duodenal papilla
- Minor duodenal papilla is where (optional) accessory duct of pancreas joins duodenum
- Enters duodenum at major duodenal papilla
- Right lobe is made up of three smaller lobes
- Hepatic portal system
- Blood coming from digestive tract would normally go directly back to the heart, but instead it goes through the liver first
- Thus, blood containing nutrients stops off at the liver before flowing to all other tissues of the body
Function
- Lobules detoxify many poisons (toxins) coming in from the digestive tract
- Waste products are secreted into bile ducts
- Lobules skim off excess glucose and other nutrients from blood before it gets to rest of body and stores them for later use
- Lobules break down old RBCs, releasing pigments from the breakdown of hemoglobin into the bile ducts
- Produces most plasma proteins
- Bile contains water, bile pigments, bile salts (fat emulsifiers), detox products, other stuff
Gall bladder
Structure
- Located below liver, attached to the bile duct system

- Hollow, muscular bag (“bladder” = “bag”)

- Cystic duct from gall bladder joins with common hepatic duct from liver to form common bile duct
Function
- Acts as an overflow reservoir for bile coming down from liver
Stores and concentrates bile
- Concentrated bile can form bile stones (gall stones)
- Contracts to release concentrated bile when there is chyme passing by
Pancreas
Structure
- 12-15 cm (length) organ cradled in the C of the duodenum, below stomach

- Most is exocrine tissue that secretes pancreatic juice into pancreatic duct
- Acinar cells are exocrine cells that produce “pancreatic juice”
- 2-3% of tissue is endocrine tissue, secreting insulin, glucagon, other hormones into blood stream
- Pancreatic islets are endocrine cells
- Pancreatic duct joins common bile duct just before it enters the duodenum

Function
- Pancreatic juice contains many substances
- Water
- Sodium bicarbonate (NaHCO3)

- CO2 + H2O <—> H2CO3 <—> HCO3– + H+
- HCO3– neutralizes stomach acid (while its H+ counterpart enters the blood to neutralize the HCO3– formed when gastric HCl is secreted)
- Trypsin & chymotrypsin — protein-digesting enzymes
- Lipases — lipid-digesting enzymes
- Amylase — carbohydrate-digesting enzyme
Digestive Physiology
Control of motility and secretion
Very complex, and still not completely understood, interaction of many different nervous and endocrine reflexes
The nervous system of the gut has been called the “second brain” because of its ability to make decisions and coordinate activity somewhat independently of the CNS
Example — phases of gastric secretion
- Cephalic phase (psychic phase)
- Anticipation of food and initial ingestion
- Parasympathetic stimulation
- Increased HCl secretion
- Increased pepsin secretion
- Increased secretion of gastrin (hormone released by stomach mucosa)
- Amplifies stimulation of HCl and pepsin secretion
- Gastric phase
- Begins when food enters stomach
- Stimuli — stretch of stomach & chemical content of food
- Gastrin secretion (especially when pH is raised when food enters)
- Increases gastric and pancreatic secretion
- Parasympathetic and gastrin stimulation of pancreatic secretion
- Protein (amino acids) and other chemicals stimulate stomach secretion
- Gastrocolic reflex (parasympathetic)
- Increased motility of lower small intestine and colon
- Gastrin secretion (especially when pH is raised when food enters)
- Stimulus — high pH in intestine (before gastric emptying)
- Increased stomach contractions and pyloric tone
- Stimulus — gastric emptying
- Opening of sphincter from small intestine into large intestine
- Intestinal phase
- Triggered by food entering small intestine
- Stimulus — distension (stretch)
- Enterogastric reflex (parasympathetic)
- Decreased gastric motility
- Enterogastric reflex (parasympathetic)
- Stimulus — low pH (stomach acid in chyme, the fluid from the stomach) & high fat
- Secretin secretion by duodenal cells
- Increased bicarbonate secretion by pancreas (raises pH)
- Decreased stomach motility
- Decreased pepsin secretion
- Decreased gastrin, thus decreased HCl secretion
- Secretin secretion by duodenal cells
Digestive enzymes (a review)
Digestive enzymes are released as proenzymes (zymogens)
- Example — Pepsinogen —> Pepsin
Digestive enzymes are hydrolases
- Promote hydrolysis of the substrate molecule
- Work only with certain substrates
Enzymes have an optimum temperature
- Peak activity near 37° C
Enzymes have an optimum pH
- Low in stomach
- Neutral elsewhere
Enzymes may be free-floating or attached
- Enzymes in “digestive juices” are free-floating
- Brush-border enzymes in intestine are attached
- Contact digestion
Absorption
Transcellular absorption — molecules are absorbed by entering a GI cell, moving through it, then leaving the cell and eventually into the blood
Paracellular absorption — molecules move through tight junctions in between cells lining the GI tract
Water and minerals 
No need for digestion
Water absorbed by osmosis
Minerals absorbed by active transport and facilitated diffusion
Carbohydrates
Polysaccharides are digested by amylase in the saliva (yeah, right) and in the intestines (pancreatic amylase) into disaccharides
Disaccharides are digested by contact digestion (with enzymes imbedded in the brush border)
Monosaccharides are absorbed by facilitated diffusion linked to active transport of sodium (sodium cotransport)
- Glucose absorption sometimes limited by availability of sodium (and vice versa)
Proteins
Proteins are denatured (unfolded) by HCl in gastric juice
Denatured proteins are broken into shorter peptides by pepsin in gastric juice
Peptides are further digested by trypsin & chymotrypsin in small intestine (pancreatic juice)
Amino acids are freed by contact digestion in brush border
Absorbed by sodium cotransport (facilitated diffusion linked to active transport of sodium)
Lipids
Lipids don’t get along well in watery fluids as do other nutrients and thus tend to form big “globs” of fat that prevent enzymes from getting to most of the lipid molecules
- Lipids must first be emulsified (broken into tiny droplets that stay separated) by bile salts (phospholipids such as lecithin)
- Form coated droplets called micelles
- Micelles are like a spherical version of a phospholipid bilayer
Lipases from pancreatic juice in the small intestine break down fats into —
- Fatty acids
- Monoglycerides
- Glycerol
- Cholesterol
Simple molecules are absorbed by simple diffusion directly across plasma membranes of brush border cells of small intestine
Fats are immediately rebuilt by the cell and packaged into vesicles called chylomicrons
Chylomicrons of fat are released by exocytosis and are carried away in the lacteals
Summary of digestive processes 

|
Location |
Process
|
Mechanism
|
Description
|
|
Mouth |
Mastication | Teeth, tongue, skeletal muscles, saliva | Mechanical — reduces size of food particles; lubricates, liquifies food |
| Carbohydrate digestion | Salivary enzyme — amylase | Chemical — hydrolysis of polysaccharides into shorter polysaccharides or disaccharides | |
|
Pharynx |
Deglutition | Skeletal muscles, slippery mucous lining | Mechanical — moves bolus of food into esophagus |
|
Esophagus |
Deglutition | Skeletal and smooth muscles, mucous lining | Mechanical — moves bolus into stomach |
|
Stomach |
Segmentation (churning) | Smooth muscles, rugae, mucus | Mechanical — forms liquid chyme, mixes enzymes with food |
| Peristalsis | Smooth muscles, pyloric sphincter | Mechanical — strong, rhythmic contractions squirts chyme pass sphincter in spurts | |
| Protein digestion | HCl, pepsin (pepsinogen activated by HCl in gastric juice) | Chemical — HCl denatures protein structure, pepsin action forms polypeptides | |
|
Duodenum |
Lipid emulsification | Bile | Mechanical — breaks large fat droplets into small droplets |
| Segmentation | Smooth muscles | Mechanical — mixes bile and other secretions with chyme | |
| Peristalsis | Smooth muscles | Mechanical — pushes chyme along rest of small intestine and into large intestine | |
| Neutralization of stomach acid | Pancreatic bicarbonate | Chemical — required for enzyme activity | |
| Lipid digestion | Pancreatic lipase | Chemical — digests lipids into fatty acids, glycerol, etc. | |
| Protein digestion |
Pancreatic proteases — Trypsin (active form) Chymotrypsin (active form) |
Chemical — digests proteins and short polypeptides into smaller chains; some amino acids formed | |
| Carbohydrate digestion | Pancreatic amylase | Chemical — digests polysaccharides into disaccharides | |
|
Jejunum, ileum |
Protein contact digestion and absorption | Intestinal peptidases on brush border | Chemical — yields amino acids at cell surface |
| Carbohydrate contact digestion | Intestinal disaccharidases on brush border | Chemical — yields monosaccharides at cell surface | |
| Absorption of simple nutrients and water | Epithelial cells lining lumen | See outline | |
| Segmentation and peristalsis | Smooth muscle | Mechanical — continued from duodenum | |
|
Large intestine |
Segmentation and peristalsis | Smooth muscle | Mechanical — continued from ileum |
| Mass peristalsis | Smooth muscle | Mechanical — descending colon contents move into sigmoid colon (usually occurs after a meal) | |
| Absorption of nutrients and water | Epithelial cells lining lumen | Less absorption than in small intestine; forms feces | |
| Defecation | Smooth muscles and skeletal muscles (GI and abdominal) | Mechanical — empties rectum |
Metabolism
Metabolic states 
The absorptive state
- During and for several hours after a meal
- Insulin
- Increased glucose uptake by cells (from blood)
- Increased glycogenesis in liver cells
- Increased lipogenesis (fat synthesis)
- Decreased lipolysis (fat breakdown) in fat cells
- Note — insulin can make you feel sluggish/sleepy, which explain the urge for a nap after a holiday meal
- Increased glucose uptake by cells (from blood)
- Continues until…
The postabsorptive state
- Starts hours after the last meal
- Glucagon
- Increased glycogenolysis (breakdown of glycogen into glucose)
- Increased gluconeogenesis (prepares lipids & amino acids for citric acid cycle)
- Increased lipolysis
- Decreased lipogenesis
- Continues to next meal; may lead to starvation if a meal is not taken
Vitamins and minerals
Vitamins are cofactors, assisting enzymes throughout the body
- Some vitamins may act as antioxidants, removing oxygen free radicals and thus their harmful effects
Minerals form ions such as sodium, potassium, calcium, etc.
- Used in a variety of ways in the body
This is a Learning Outline page.
Did you notice the EXTRA menu bar at the top of each Learning Outline page with extra helps?
Last updated: October 22, 2019 at 14:01 pm