Learning Outline
Blood
A&P 2
Overview of blood tissue
Introduction
Blood connects all the various tissues of the body
- Blood is part of every organ and every system
- Is a “connective” tissue in a functional sense
- Will relate directly to remaining topics of this course: cardiovascular, respiration, etc.
Structure
Connective tissue with liquid matrix (plasma)
Cells and cell fragments are also called formed elements
Flows within cardiovascular system (heart and blood vessels)
Blood volume
- 71 ml/kg (70 kg adult male would have about 5,000 ml total blood volume)
- About 55% is fluid and about 45% formed elements
Function
- Transportation of molecules within the internal fluid environment
- Exchange between tissues and between internal/external environment
Secondary functions
- Immunity — defense
- Thermoregulation — acts as “radiator fluid”

- Fluid volume homeostasis
- pH homeostasis
Blood and cardiovascular problems are a major health concern ![]()
![]() FYI Interested in learning more? I recommend this book for further reading—Five Quarts: A Personal and Natural History of Blood
FYI Interested in learning more? I recommend this book for further reading—Five Quarts: A Personal and Natural History of Blood
Formed elements – overview
Hematopoiesis
Hematopoiesis — formation of new blood cells
- All are descended from stem cells in red marrow (myeloid tissue)
- Divide into “lines” of daughter cells, each line producing different groups of blood cells (differentiation)
Main types
- Platelets — clotting cells
- Red blood cells — carry blood gases
- White blood cells — immune cells
![]() FYI Cells of the blood is a visualization of each type of blood cell.
FYI Cells of the blood is a visualization of each type of blood cell.
Blood cell types
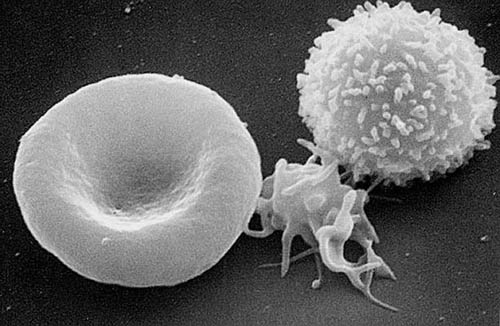
Red cell (left), platelet (center), white cell (T lymphocyte; right). SEM
Red blood cells
Name
Also called RBCs or erythrocytes [lit. “red cells”]
Number
4-6 million per cubic mm of blood (RBC count)
45% of total blood volume (packed cell volume [PCV] or hematocrit)
 |
Hematocrit (PCV “packed cell volume”) |
Shape
- 7 micron (µm) diameter
Deformable
- PGE increases deformability
- PGE2 decreases deformability
Crenation — shrinkage from water loss (as in a hypertonic solution)
Cytoplasm
Organelles few in number (no nucleus)
- Lost during development
Contain about 300 million molecules of hemoglobin (Hb)
- Quaternary protein made of four polypeptides, each with an iron (Fe) containing heme group in the center (of each folded polypeptide)
- Oxyhemoglobin (HbO2) forms when O2 combines with heme groups
- Carbaminohemoglobin (HbCO2) forms when CO2 combines with amino acids in polypeptide chains
- Anemia — less normal hemoglobin than usual (< 10g/100ml)
Life cycle
RBC hematopoiesis
- Erythropoiesis
- Stem cells (hemocytoblasts) in red bone marrow (myeloid tissue)
- Stimulated by hormone erythropoietin (EPO), which is formed in kidney in response to low O2 delivery to tissue cells (tissue hypoxia)
- Example: hematocrit (RBC%) goes UP when you stay at higher elevations, where O2 concentration in air is lower
- Requires: vitamin B12 (and intrinsic factor), folic acid (folate or vitamin B9), iron (Fe)
- Blood doping
- Add blood to increase hematocrit, and thus O2 capacity
- Add EPO to increase RBC production, increasing O2 capacity
RBC destruction
- Last about 4 months (can’t repair themselves because they lack nuclei)
- Run through “obstacle courses” in spleen and liver and aged cells break apart
- Macrophages eat them
- Globin (polypeptide) part is reduced to amino acids and recycled
- Heme is stripped of its iron, which is recycled
- Remain part of heme is converted to bilirubin (yellowish pigment that gives plasma its characteristic “straw” color)
Formation of blood cells
The RBCs in this diagram look strange. What is odd about them?
Blood types
Blood typing is the earliest form of “tissue typing”
- Karl Landsteiner discovered ABO system (1902), Rh system (1904) and later other blood types, for which he won a Nobel Prize
Based on glycoprotein markers (antigens) on surface of RBCs
ABO system looks for A or B markers (antigen)
- Type A — antigen A only
- Type B — antigen B only
- Type AB — both A and B antigens
- Type 0 — neither A nor B antigen present
Rh (D antigen) system (named for Rhesus monkeys)
- Rh positive — Rh (D) antigen present
- Rh negative — Rh antigen absent
Other systems of blood typing exist —looking for different antigens (markers)
Read over textbook material on practical applications of this theory
White blood cells
Name
White blood cells are also called WBCs or leukocytes [lit. “white cells”]
Number
Less than 1% of whole blood
- 5,000 – 10,000 per cubic mm of blood (WBC count)
- Leukopenia — abnormally low WBC count
- Leukocytosis — abnormally high WBC count
- Often observed in leukemia (tumor of WBCs)
Life cycle
Leukopoiesis is development of new WBCs
- Produced in bone marrow, but some migrate to lymphoid tissue for most of development (lymphoid tissue is found in lymph nodes, thymus gland, spleen, liver, elsewhere)
Lifespan is uncertain, perhaps 3 days to a year, depending on type
Location
Not confined to blood stream
Chemotaxis — move toward chemical attractants (chemotactic factors)released at site of injury/infection ![]()
![]()
Diapedesis — move between, or even through, other cells to get to their target

Functions
Immune functions of various sorts, for example
- Phagocytosis
- Release of cell toxins
- Release of immune function regulators
- More on immunity later (see Chapter 21)
Types
Types distinguished by how they stain with Wright’s stain —a mix of different cell stains
Differential WBC count — distinguished how many of each type of WBC in sample
Granulocytes (look granular when stained)
- Basophils (stain with the basic stain in Wright’s mixture)
- Eosinophils (stain with the acid stain called eosin)
- Neutrophils (stain with a neutral stain)
Agranulocytes (do not look granular when stained)
- Lymphocytes (small—8 microns (µm); develop in lymphoid tissue)
- Monocytes (large—15-20 microns (µm); develop into macrophages)
Platelets
Name
Also called thrombocytes
Structure
- 2-3 microns (µm)
Do not have nuclei
Life Cycle
Thrombopoiesis is development of new platelets
- Formed in red marrow
- Fragments of larger ancestor cells
- Megakaryoblasts develop into megakaryocytes, which each release 2-3 thousand tiny platelets
Life span — about a week
Regulated by hormone thrombopoietin
Function
Play important role in stopping leaks in vessels
More on this role follows
Stopping leaks
Overview
Hemostasis — process of stopping leakage of blood
Coagulation — part of hemostasis, it involves a complex process that eventually forms a blood clot to stop leaking blood
- Also called the clotting mechanism
- Involves a cascade of processes in which one step triggers another, then another
- Opportunities at various steps to enhance or inhibit process
Process
Injury to blood vessel occurs, exposing collagen fibers in wall of blood vessel
Platelet plug forms (short-term fix)
- Platelets have net positive charge on outside surface (recall membrane potentials)
- Collagen has slightly negative charge, so platelets are attracted to site of injury
- Platelets release thromboxane, making them sticky and also calling in more platelets (chemotaxis in action)
Blood clot (thrombus) forms (medium-term fix)
- Thromboplastin is released from platelets (intrinsic mechanism) and damaged tissue cells (extrinsic mechanism)
- This is an example of redundancy . . . often seen in safety mechanisms
- Triggers conversion of prothrombin (plasma protein) into thrombin
- Thrombin converts fibrinogen (plasma protein) into fibrin
- Fibrin is stringy protein that traps cells and tightens to form a rather solid mass (clot)
Blood clot dissolves as new tissue replaces injured tissue (long-term fix)
- Dissolution of clot starts when clot is formed (pre-programmed dissolution)
- Otherwise, thrombus may break off and float away (an embolus) and block blood flow in brain, heart, lungs —-killing you
- Plasmin is chemical largely responsible for dissolving fibrin
Clotting mechanism requires many different chemicals (clotting factors) ![]()
- Clotting factors are often identified by Roman numerals (Factor I, Factor II, etc.)
- If any one factor is missing (or abnormal), hemophilia (clotting disorder) is likely to result
Plasma
Location
Extracellular liquid part of blood tissue
Composition
See diagram in text for specific proportions
Mostly water
Plasma protein
- Albumins “thicken” blood and because they are relatively impermeant, hold water in the blood by way of osmosis
- Globulins include immunoglobulins (Ig) —antibodies— for immunity
- Fibrinogen is a protein needed for blood clotting
Other solutes
- Ions such as Na+, Cl–, K+, Ca++, H+, HCO3–, and others
- Nutrients such as glucose, fatty acids, amino acids
- Waste products such as
- Lactic acid from anaerobic processes
- Urea from breakdown of amino acids used in cellular respiration
- Yellowish pigments from breakdown of hemoglobin (from old red blood cells)
- Gases such as CO2 and O2
- Regulatory substances such as hormones, prostaglandins, clotting factors
Blood serum (pl. sera) — plasma without the clotting factors
Last updated: December 21, 2020 at 20:17 pm
This is a Learning Outline page.
Did you notice the EXTRA menu bar at the top of each Learning Outline page with extra helps?