Learning Outline
Muscular System
This outline focuses on the general anatomy and physiology of muscle organs. Names, locations and actions of specific muscles are not covered here.
For an optional overview of muscles and their actions click here.
Muscular System Overview
Includes organs comprised mainly of skeletal muscle tissue and connective tissue
General functions
Movement
Heat production
Posture
Body shape
Skeletal muscle organs
Overview
Made up of muscle fibers, nerves, blood vessels and connective tissues
Functional characteristics of muscle fibers
- Excitable — respond to stimuli by fluctuation of voltage in membrane
- Contractile — can shorten in length
- “Contraction” can also refer to steadily resisting a load—not always shortening in length
- Extensible — can stretch (compliance)
- Muscles can exert force while extending, as in slowly lowering a heavy weight in your hand
- Elastic — can recoil to starting length after being stretched
General principles of functional anatomy of the muscle organ
Skeletal muscle organs contract (not expand) with force
Skeletal muscle organs act in teams
- Antagonistic (opposing) pairs
- Prime mover and antagonist must coordinate contraction/relaxation
- Synergists (synergy = when a combined effect is greater than the expected sum of effects)
- Agonists (same/similar action as prime mover)
Skeletal muscles attach to the skeleton
- Origin — attached to “stationary” bone
- Insertion — attached to “mobile” bone
Fibrous connective tissue wraps and compartmentalizes muscle fibers
- Endomysium wraps single fibers
- Perimysium wraps bundles or fascicles
- “Fascicle” from fascis = gang (of fibers) and -iculus = small
- Epimysium wraps whole organ
- Combined fibrous tissue extends beyond muscle tissue on each end, forming tendons that connect to bones
- Aponeurosis — a tendon in the form of a broad, flat sheet
- Aponeuroses (plural)
- Tendon sheath — double-walled tube of synovial membrane that reduces friction
Required— read carpal tunnel syndrome box in Chapter 11 (p. 331)
- Aponeurosis — a tendon in the form of a broad, flat sheet
- Loose fibrous connective tissue between and around muscle organs is deep fascia
- Myofascial meridian — long, continuous chain formed by linked muscles and fascia and which maintain posture and provide movement
- Read A&P Connect article Whole-Body Muscle Mechanics in your Evolve resources
Hernia — “rupture” or protrusion (sticking out) through a wall
- Inguinal hernia — protrusion through inguinal canal
- Femoral hernia — protrusion through femoral ring
- Umbilical hernia — protrusion through umbilicus (navel)
- Hiatal hernia — protrusion through hiatus (opening) of diaphragm
Required: read article from A&P Connect called Hernias in Chapter 11 Resources at Evolve website
Review Mini Lesson: Fascial System
Muscle fiber structure
Basic structures
Sarcolemma = plasma membrane
- T tubules (transverse tubules) are inward extensions of the sarcolemma, like tunnels through a mountain
Sarcoplasm = intracellular material
Sarcoplasmic reticulum (SR) = special form of smooth ER with Ca2+ ion pumps that allow SR to store Ca2+
- Important principle you will use throughout life (and into the next) — “cells HATE calcium”
- SR is up against both sides of each T tubule, forming a triad
Myofibrils
Cylindrical units of the cytoskeleton made up of microfilaments (= myofilaments)
Sarcomeres — repeating, overlapping pattern of thin and thick [myo]filaments in the myofibril
- Each sarcomere extends from one Z disk to the next
- A Z disk (old name: Z line) is a network of fibers formed where the thin filaments are anchored together (looks like a zigzag line from the side)
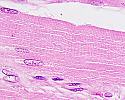 |
Muscle micrograph. The striated pattern of the human sarcomeres is clearly visible in this specimen (click to enlarge) from Blue Histology |
Thick filaments
- Mostly myosin, a golf-club-like protein molecule with a hinged “head”
- Molecular motor
- Myosin loves actin (has a binding site that “fits” actin’s binding site)
- Myosin head has a “battery holder” for ATP, which energizes the head —allowing the head to “cock back” like a sling shot
Thin filaments
- Mostly actin, bead-like protein molecules strung together like a string of pearls (actin returns myosin’s affections)
- Tropomyosin is a strand of protein that blocks actin’s active sites, preventing an actin-myosin rendezvous
- Troponin is a “glob” of protein that holds tropomyosin in its blocking position (otherwise, myosin’s hinged head would simply knock tropomyosin out of the way to get to its true love, actin)
- Troponin has a crush on Ca2+, which will “never” be fulfilled because all the Ca2+ is in the SR or outside the muscle fiber (that is, troponin has an open binding site for Ca2+)
Muscle fiber contraction
A love story?
Myosin and actin want each other (can’t get together because of tropomyosin and troponin)
Troponin wants Ca2+ but Ca2+ is unavailable
Scenes of the unfolding love story
- Motor neuron releases acetylcholine (Ach; a neurotransmitter) at neuromuscular junction
- Ach induces an impulse (voltage fluctuation) in the sarcolemma
- Impulse travels along the sarcolemma and through the T tubules
- Impulse in T tubules “zaps” the SR, which suddenly releases its Ca2+
- Ca2+ diffuses throughout sarcoplasm
- Troponin’s dreams are realized when Ca2+ binds to troponin
- In the heat of passion, troponin now twists around —pulling tropomyosin out of its blocking position
- Myosin heads can now reach actin’s binding sites and, well, you know what happens then
- Myosin’s head pulls actin toward the center of the sarcomere (then grabs another and another actin)
- This causes the thin filaments to slide past the thick filaments, shortening the sarcomere
- “Sliding filament model” of muscle fiber contraction
Sliding Filament Model animation
From https://course1.winona.edu/sberg/Free.htm used by permission
- In the mean time, SR has recovered its wits and is again pumping Ca2+ into storage
- Ca2+ is thus pulled away from troponin, which flips back to its position and pulls tropomyosin back into its blocking position
- Myosin is now blocked from reaching another actin; the contraction stops
Myosin and ATP
- ATP binds to a myosin head and breaks into ADP + P
- Released energy is used to “cock back” the myosin head
- If actin is available, the myosin head will bind to actin and pull
- If actin is unavailable, the myosin head will wait (cocked back and ready to go) until actin becomes available
- A new ATP is now needed to get myosin to release from actin and cock back again
- At death, no ATP is available and the myosin & actin are “stuck” in place (rigor mortis = stiffness of death)
Power stroke of myosin head.
From https://course1.winona.edu/sberg/Free.htm used by permission
From https://course1.winona.edu/sberg/Free.htm used by permission
Summary of the story
- Excitation
- Contraction
- Relaxation
Excitation-contraction coupling refers to the fact that these two processes (excitation and contraction) are linked [coupled]
Not required — See p. 166 in Survival Guide For Anatomy And Physiology: Tips, Techniques And Shortcuts
for a summary of the “muscle love story”
For an interesting alternate hypothesis about how muscle fibers work, I highly recommend the book Cells, Gels and the Engines of Life by Gerald Pollack
Energy for contraction
Energy sources
ATP — from aerobic (slow) and anaerobic (fast) respiration
Creatine phosphate (CP) — “backup battery” for quick recharging of ATP
More on this (a little) later
Fiber types
Overview
- Slow fibers specialized for endurance; rely mainly on aerobic respiration
- Fast fibers specialized for quick, strong contractions; rely mainly on anaerobic respiration
Specific types
- Type I— slow oxidative [red muscle]
- Predominate in soleus muscle
- Postural muscles — slow but efficient; fatigue resistant
- Abundant capillaries, high myoglobin content
- Type IIa — fast oxidative [red muscle]
- Predominate in gastrocnemius muscle
- Intermediate characteristics — moderately fast and moderately fatigue resistant
- moderate capillary supply and myoglobin content
- Type IIx — fast glycolytic [white muscle]
- Also called Type IIb
- Predominate in muscles of eyes and fingers
- Rely heavily on glycolysis; high glycogen content
- Fast but fatigue easily; brief, powerful contractions
Muscle organs are mix of types
- Organs that often perform quick powerful contractions have a high proportion of white fibers
- Organs for posture have a high proportion of red fibers
- The proportions can change when one shifts their types of activities (as in aging)
Cellular Respiration
Overview
The key here is focusing on “what’s really happening” without getting bogged down in the details of the biochemistry
- What’s really happening:The cell transfers energy from fuel molecules eventually to ATP
You should also print out the Getting Energy review outline and use it to help you understand these concepts.
Basic definitions
Metabolism — body chemistry
- Catabolism — chemistry that breaks big molecules into small ones
- Anabolism — chemistry that builds small molecules into big ones
- Metabolic pathway — series of chemical reactions, one leading to the next, and so on
Respiration — literally “re-breathing” and refers to bringing in oxygen (O2) and releasing carbon dioxide (CO2)
- Cellular respiration — chemical process in cells that uses oxygen and gives off carbon dioxide, really referring to energy transfer
- Aerobic pathway — respiration pathway that requires oxygen
- The term “aerobic respiration” is often used for this pathway
- Anaerobic pathway — respiration pathway that requires no oxygen
- The term “anaerobic respiration” is often used for this pathway. However, biologists recognize that glycolysis is technically a type of fermentation and not true respiration. We will use the term “anaerobic respiration” in our course.
Coenzyme — coenzymes “help” enzymes
- In this story, it is helpful to think of coenzymes as “escorts” that move molecular fragments from one chemical pathway to another
- Main examples
- NAD (nicotinamide adenine dinucleotide)
- FAD (flavin adenine dinucleotide)
Summary of chemical changes
C6H12O6 + O2 H2O + CO2 + energy (in ATP)
[this equation is not balanced]
Step 1 — Glycolysis
Breaks glucose (C6) into two pyruvic acids (2 C3) and releases energy
Enough energy is released for 2 ATP molecules
Anaerobic
Occurs in cytosol outside of mitochondria
Step 2 — Transition reaction
If pyruvic acid is to continue, it enters the mitochondrion and one carbon is removed —forming Acetyl (C2)
Coenzyme A (CoA) temporarily binds to acetyl and escorts it into the citric acid cycle
This begins the aerobic process (although O2 will not actually be used until later, the molecule will not enter this pathway until and unless O2 is there at the end of the line)
Step 3 — Citric Acid Cycle
Citric Acid Cycle also known as Krebs Cycle or TCA Cycle
Acetyl rides this “ferris wheel” where it is broken apart, releasing its energy
The Cs and Os simply fall away, forming the waste CO2
Most of the energy released in the form of energized electrons from H (the H+ proton also tags along for the trip)
- The high-energy electrons (and H+) are picked up by coenzymes NAD and FAD and escorted to the electron transport system (ETS)
 Hans Adolph Krebs shared the 1953 Nobel prize in Physiology or Medicine for his discovery of the citric acid cycle. At the prize ceremony, the presenter stated, Hans Adolph Krebs shared the 1953 Nobel prize in Physiology or Medicine for his discovery of the citric acid cycle. At the prize ceremony, the presenter stated,
“It was Krebs who discovered how these individual reactions are linked to each other in a cyclic process. He brought us a clear understanding of the essential principle of how the released energy is used for the building up processes which take place within the cell.” (The prize was shared with Fritz Albert Lipmann for his discovery of the role of Coenzyme A.) |
 The ferris wheel is one model for how the citric acid cycle (Krebs cycle) works.Coenzyme A escorts a molecule of acetyl (obtained from glycolysis) into the cycle, just as the ride operator escorts riders onto the ferris wheel. Instead of getting into a car, the acetyl molecule is transferred to a “carrier” molecule to form citric acid. As this combined molecule completes the cycle, the “passenger” is broken apart and pieces “fly off” and away from the cycle. The “car” returns empty, ready to pick up another “passenger.” Some of the “flying pieces” are high-energy electrons that are escorted to the ETS by coenzymes and their energy eventually transferred to ATP. The ferris wheel is one model for how the citric acid cycle (Krebs cycle) works.Coenzyme A escorts a molecule of acetyl (obtained from glycolysis) into the cycle, just as the ride operator escorts riders onto the ferris wheel. Instead of getting into a car, the acetyl molecule is transferred to a “carrier” molecule to form citric acid. As this combined molecule completes the cycle, the “passenger” is broken apart and pieces “fly off” and away from the cycle. The “car” returns empty, ready to pick up another “passenger.” Some of the “flying pieces” are high-energy electrons that are escorted to the ETS by coenzymes and their energy eventually transferred to ATP. |
Step 4 — Electron Transport System (ETS)
Also known as Electron Transport Chain (ETC)
High-energy electrons (and H+) are dropped off at molecules in the cristae
The electrons are shuttled from molecule to molecule losing their energy as they go (passed like a hot potato, eventually “cooling off”)
The energy lost by electrons is used to pump the protons (H+) into the intermembrane space, like water behind a dam
As the protons flow back through the dam (down their concentration gradient), this powers the “phosphorylation of” or “adding phosphate to” ATP (oxidative phosphorylation)
The electrons unite with their protons, forming H2 which is explosive
- H2 is immediately “burned” by O2, forming waste H20
 The Hindenburg zeppelin, a blimp filled with hydrogen gas (H2), exploded as it attempted to land at Lakehurst NJ near New York City in May, 1937.Although the explosion is now thought to have been caused by lightning that set off an explosive powdered aluminum coating on the skin of the balloon, this disaster was originally thought to be primarily an explosion of hydrogen gas—thus effectively ending the age of the H2 zeppelins. The Hindenburg zeppelin, a blimp filled with hydrogen gas (H2), exploded as it attempted to land at Lakehurst NJ near New York City in May, 1937.Although the explosion is now thought to have been caused by lightning that set off an explosive powdered aluminum coating on the skin of the balloon, this disaster was originally thought to be primarily an explosion of hydrogen gas—thus effectively ending the age of the H2 zeppelins.
In aerobic cellular respiration, H2 produced in the mitochondria (ETS) is oxidized immediately before it can build up to an explosive amount. Thus the need for O2. (Click here to see more on the Hindenburg disaster, including video of the disaster.) |
Total Energy Yield
A total of 36-38 ATPs are available from aerobic respiration
- Only 2 ATPs become available in the anaerobic pathway
See the ATP Yield Table for clarification
Anaerobic Option
Lactic acid
- Forms when pyruvic acid does not enter the aerobic pathway
- Happens when not enough oxygen or when energy is needed more quickly than aerobic respiration can handle
- Later converted back to glucose
- Requires O2, hence the origin of the term “oxygen debt” in anaerobic respiration
- EPOC — excess post-exercise oxygen consumption is actually caused by the entire set of events that restore muscles to the “resting state” after exercise (restoration of fat storage, etc.)
Formation of lactic acid means that the molecules have followed the “anaerobic pathway”
Fuel sources 
Glucose primarily (or anything that can be coverted to glucose)
Glycogen (stored in muscle fibers, not most other cells)
Other fuels converted to some form of glucose (lipids, proteins)
Not required — click here for the full chart of the Krebs Cycle —if you dare!
Muscle organ contraction
Motor unit
Motor unit — group of muscle fibers all connected to the same motor neuron, thus acting as a unit
Different levels of contraction in a muscle organ can result from recruitment of different numbers of motor units
Myography
Myography produces a wave-like picture of muscle organ contraction called a myogram
Twitch contraction — single, brief contraction in response to a single stimulus
- One or more motor units contracting in unison
- Three phases — latent, contraction, relaxation phase
Treppe (staircase effect)
- Increase in the strength of contraction in the first few of a series of contractions
- Due to increasing warmth, more diffusion of Ca2+ and other factors
Wave summation (tetanus) — sustained contraction
- Tetanus is normal
We are not talking about the rare “tetanus” disease or “lockjaw” which is involuntary muscle rigidity caused by toxins produced when the bacterium Clostridium tetani infects a deep wound
- Most normal contractions are tetanic (not single twitches)
- What produces tetanus?
- Relays of motor units (or groups of motor units) result in a sustained contraction
- Ca2+ builds up and remains available to myosin when stimulations are frequent
- Complete tetanus — no relaxation between peaks of myogram
- Incomplete tetanus — some relaxation between relays (usually, fatigue causes some relays to “drop out” because they are tired)
Muscle tone
Muscle tone — continuous, low-level sustained (tetanic) contraction of any (or all) muscle organ(s) —the starting point for stronger contractions
Flaccidity — abnormally low tone, as in paralysis or immobility (cast)
Spasticity — abnormally high tone, as in CP or Parkinsonism
Fibrillation
Fibrillation — asynchronous, uncoordinated contractions within a muscle organ
Abnormal; occurs with fatigue, chemical imbalance
- Produces no effective movement
Spectrum of muscle organ contractions
Isotonic contraction — same tension; shorter length
- Mobilizes body parts
- Two types
- Concentric contraction — muscle shortens (as in lifting a load)
- Eccentric contraction — muscle lengthens while contracting (as in setting down a load without dropping it)
Isometric contraction — increased tension; same length
- Stabilizes body parts (as in maintaining posture)
Most muscle contractions are somewhere between two ends of spectrum
Graded strength principle
Recruitment of more or less motor units
Length
- Generally, the greater the starting length, the greater the strength
Metabolic condition
- For example: temperature, Ca2+ availability, ion balance across membrane, ATP availability, etc.
Stretch reflexes
Skeletal muscles contract only if stimulated
Smooth and cardiac muscles, however, may contract rhythmically without external stimulation
Muscle size
Atrophy — disuse atrophy is a reduction in muscle size resulting from lack of use
Hypertrophy — increase in muscle size resulting from maximal use, especially heavy-load-bearing contractions
Stretching muscles can cause a rapid increase in the length of myofibrils
 |
This sketch from Leonardo da Vinci’s notebook shows contraction of the biceps brachii muscle and flexion (bending) of the elbow. How do we know whether it’s isometric or isotonic contraction? Could it be both?
(Click the image to enlarge it) To see an animated cartoon of the muscle’s contraction click here. |
Readings, References, & Resources
A&P Core
Betts, J. G., DeSaix, P., Johnson, J. E., Korol, O., Kruse, D. H., Poe, B., Wise, J. A., Womble, M., & Young, K. A. (2013). Anatomy and physiology.
Khan Academy. (n.d.). https://www.khanacademy.org/science/health-and-medicine
Patton, K. T. (2013). Survival Guide for Anatomy & Physiology. Elsevier Health Sciences.
Patton, K. T., Bell, F. B., Thompson, T., & Williamson, P. L. (2022). Anatomy & Physiology with Brief Atlas of the Human Body and Quick Guide to the Language of Science and Medicine. Elsevier Health Sciences.
Patton, K. T., Bell, F. B., Thompson, T., & Williamson, P. L. (2023). The Human Body in Health & Disease. Elsevier Health Sciences.
Patton, K. T., Bell, F. B., Thompson, T., & Williamson, P. L. (2024). Structure & Function of the Body. Elsevier Health Sciences.
Topic Focused
Coming soon!
Last updated: February 16, 2025 at 17:11 pm