Learning Outline
Urinary System
A&P 2
Importance of the Urinary System
Urinary system filters blood and thus helps to maintain
- Fluid/electrolyte balance
- Acid/base balance
Urinary system produces urine, but as a side-effect—NOT the primary function of the urinary system!
Fluid/Electrolyte homeostasis
Fluid compartments
“Compartments” are a convenient way to picture the fluids of the body
Extracellular fluid (ECF) compartments (about a third of all body fluids)
- Interstitial fluid (IF) — fluid between tissue cells
- Plasma — fluid portion of the blood
- Lymph — fluid in lymph nodes and vessels
- Other — CSF, joint fluid, eyeball fluid, and so on
Intracellular fluid (ICF) compartment (about 2/3 of all body fluids)
- Includes cytosol of all cells
Fluid homeostasis
Balance is maintained for good health
Leaks prevented by blood clotting
Excesses or deficiencies of fluids in one tissue are simple “moved around” or “rationed” among all the other tissues by the plasma
- Thus, no one tissue is very far out of balance (under- or overhydrated)
- Instead, ALL tissues are out of whack just a little bit
Overall input and output of water to/from the body can be adjusted
- Input
- Primarily adjusted by the thirst mechanism
- Liquid ingestion
- Ingestion of moist solids
- Osmoreceptors in the brain work with the hypothalamus to regulate the thirst mechanism
- Subfornical organ (SFO) in roof of 3rd ventricle has osmoreceptors
- Additional osmoreceptors in ADH-producing cells of hypothalamus
- Metabolism (H2O is a product of cellular respiration) supplies some water, but is not really adjusted to maintain water balance
- Primarily adjusted by the thirst mechanism
- Output
- Primarily adjusted by changing output (volume) of urine from the kidneys
- Also affected by these other outputs that are not adjusted to maintain water balance
- Respiratory (loss during expiration)
- Digestive (feces)
- Skin (sweating)
- Usually easier to adjust output than input because input requires availability of water (which is not under physiological control)
- Fluid balance regulated by hypothalamus
Electrolyte homeostasis
Electrolytes dissociate to form ions when dissolved in water
- Cations are positive ions
- Anions are negative ions
Distribution of various electrolytes differs between the intracellular fluid compartment and the extracellular fluid compartment
- Cellular mechanisms of balance— sodium-potassium pump, calcium pump, other ion pumps
- Extracellular mechanism of balance — urinary system
Functional anatomy of the urinary system
Macroscopic (gross) anatomy
Kidneys
- Location — back of abdominal cavity at top of lower back (lumbar region)
- Structure — bean-shaped paired organs covered with fibrous capsule
- Size — from approx. 7.5 cm x 2.5 cm up to about 11.25 cm x 5 cm
- Hilum
- Medial “notch” where vessels/tubing enter/exit the kidney
- Capsule
- Outer wall of fibrous tissue
- Cortex (a.k.a. renal cortex)
- Outer region of kidney tissue
- Medulla (a.k.a. renal medulla)
- Inner (deeper) region of kidney tissue
- Renal pyramids are cone-shaped pieces of kidney tissue that point toward the medial opening of the kidney
- The tips of the pyramids are called renal papillae and have many tiny openings for the release of urine from the pyramids
- Tissue between the pyramids is called renal columns
Plumbing
- Urine from renal papillae is collected in branchlike tubes that drain into a basin called the renal pelvis
- Branches that lead into the basin are called (major and minor) calyces (singular calyx, literally “cup”)
- Ureter drains urine from the pelvis of the kidney
- Urinary bladder collects urine from ureters
- Stores urine until a socially acceptable time and place to urinate
Lined with transitional epithelium capable of stretching greatly without damage
- Trigone — 3-cornered floor of bladder
- Posterior corners — left and right ureters enter
- Anterior corner — urethra exits
- Capacity — about 150 cc (more or less)
- Cyst- is the word part that means “bladder”
- Urethra drains urine from bladder to outside of body
- Micturition (urination, voiding urine, pissing, peeing)
- Detrusor muscle (bladder wall) increases rhythmic contractions as bladder fills (intrinsic and parasympathetic reflexes)
- Internal urethral sphincter relaxes (parasympathetic reflex)
- External urethral sphincters contract (somatic motor reflex)
- When filled to about 250 ml AND in a socially acceptable time and place . . .
- External urethral sphincters relax (voluntary, thank goodness)
- Voluntary nervous control not possible during infancy and into toddler stage (or later)
- Also may be lost later in life (due to injury to muscles or nerve pathway; stress)
- Voluntary nervous control not possible during infancy and into toddler stage (or later)
- Primary Principle of Pee — urine flows down a pressure gradient
- Contractions of bladder wall increase urine pressure in bladder
- Some abdominal muscles contract to increase abdominopelvic pressure
- External urethral sphincters relax (voluntary, thank goodness)
- Detrusor muscle (bladder wall) increases rhythmic contractions as bladder fills (intrinsic and parasympathetic reflexes)
- Plumbing issues
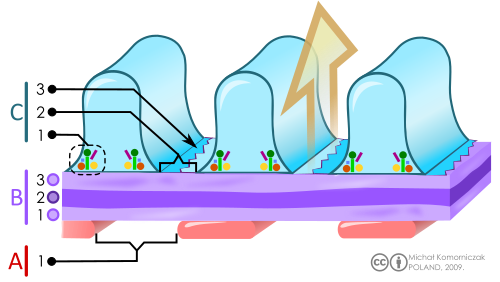
Microscopic anatomy
Overview of microscopic plumbing
- Nephron
- Renal corpuscle
- Glomerulus
- Bowman capsule
- Renal tubule
- Proximal convoluted tubule (PCT)
- Henle loop
- Descending limb (DLH)
- Thin ascending limb (tALH)
- Thick ascending limb (TAL)
- Distal convoluted tubule (DCT)
- Renal corpuscle
- Collecting duct (CD)—shared by several different nephrons
- Fluids
- Blood — plasma is the main player here
- Filtrate — material that forms in the tubules
- Urine — what we call the filtrate after it leaves the tubules and ducts of the kidney
- Sometimes filtrate is called urine, but that is not precisely accurate
Renal corpuscle — glomerulus and Bowman capsule
- Glomerulus
- Ball-like network of capillaries (glomerular capillaries)
- Supplied by an afferent arteriole
- Drained by a smaller efferent arteriole (which leads to a second network of capillaries after the glomerulus)
- Endothelial cells of the glomerular capillary wall have fenestrations or pores (like White Castle hamburgers)
- Fenestrated wall acts as a filter, keeping blood cells and proteins in blood and allowing water and small solutes to filter out of blood
- Mesangial cells — support cells between the capillaries
- Ball-like network of capillaries (glomerular capillaries)
- Bowman capsule (glomerular capsule)
- Surrounds glomerulus like a hollow cup
- Inner (visceral) wall of capsule adheres to outer walls of glomerular capillaries
- Cells are spider-like cells called podocytes (lit. “foot cells”)
- Podocytes have pedicels or “little feet” that interlock like a zipper to form a filtration membrane with slits (filtration slits)
- Filtration slits are covered with a thin fibrous membrane (slit diaphragm)
- Acts as second layer of filter
- Surrounds glomerulus like a hollow cup
- Filtration membrane
- Glomerular capillary wall
- Basement membrane (shared)
- Inner (visceral) wall of Bowman capsule
Proximal convoluted tubule (PCT)
- Convoluted means it has a lot of twists and turns
- Proximal refers to the fact that it is close to the beginning of the nephron
Henle loop (nephron loop or loop of Henle)
- Hairpin turn of the nephron, dipping far down into the medulla (from the renal cortex, where most of the nephron is located)
- Has a thin descending limb followed by an ascending limb
- The ascending limb has a thin segment followed by a thick-walled segment
- Thin ascending limb of Henle (tALH)
- Thick ascending limb (TAL)
- The ascending limb has a thin segment followed by a thick-walled segment
Distal convoluted tubule (DCT)
- Drains filtrate from the Henle loop
- Juxtaglomerular apparatus
- Found near glomerulus, where afferent arteriole touches DCT
- Made up of
- Macula densa (thick part of DCT wall)
- Juxtaglomerular (JG) cells near afferent arteriole
- Secretes renin when afferent arteriole BP decreases
- Promotes RAAS (renin-angiotensin-aldosterone system) — covered in previous topics, and reviewed again below
Collecting duct (CD)
- Drains filtrate from distal tubules of several different nephrons
- Many collecting ducts converge at the renal papillae and release urine from the kidney tissue
Blood supply
- Afferent arteriole -> glomerulus -> efferent arteriole -> peritubular capillaries (includes vasae rectae)
- Peritubular capillaries surround the entire nephron (except the Bowman capsule, which has the glomerulus instead)
- Vasa recta (lit. “vessels at a right angle”) conduct blood down, then up, the outside of the Henle loop [singular “vas rectum”]
Two types of nephron
- Cortical nephrons are further to the outside and have short Henle loops that do not reach into the medulla
- Juxtamedullary nephrons are mostly in the cortex close to the medulla and have long Henle loops that dip far into the medulla (from the cortex)
Urinary physiology
The basics
The basics — balancing of blood plasma & formation of urine
- Importance — adjusts fluid and electrolyte balance of blood (thus, entire body)
- Three essential functions
- Filtration
- Reabsorption
- Secretion
- Excretion — exit of what remains after the above functions
- Excretion = Filtration – Reabsorption + Secretion
Bowman capsule
Ultrafiltration (from glomerulus)
About 20% of plasma flow (most is later reabsorbed)
- Adds up to about 50 gallons of filtrate per day (that’s not a mistake—50 gallons that can potentially be released as urine!) (125 ml/min)
Glomerular filtration rate (GFR) influenced by blood pressure
- Effective filtration pressure (EFP) is needed to maintain sufficient GFR
Proximal tubule
Reabsorption and secretion
Reabsorption of most of Na+ , Cl– and H2O
- Sodium is transported actively
- Chloride and water follow passively
Reabsorption of other solutes (passive – or actively cotransported with Na+)
- Glucose transport maximum (Tmax)
- Co-transported with Na+
- Na+ is pumped from back of tubule cell, drawing more Na+ in through front of tubule cell (by way of passive carriers)
- Carrier mechanism carry glucose at the same time
- Thus, the active-transport driven movement of Na+ brings glucose “along for the ride”
- Largest amount of glucose that can be transported at once
- Determined by how many passive carriers for glucose you have (the more carriers, the higher the transport maximum)
pH adjustment (H+ secretion)
About half of the urea is reabsorbed passively here
Henle loop (nephron loop)
Creates/maintains osmotic gradient between medulla and cortex
Medulla’s IF maintained at high saltiness
- “saltiness” is measured as osmolality (units — mOsm)
- high osmolality = high saltiness = high osmotic pressure (tendency to gain water by osmosis) = hypertonic
- Most body fluids are isotonic to each other at about 300 mOsm
- Medullary IF goes up to about 1200-1400 mOsm
Salt actively removed by ascending limb
- This is the countercurrent multiplier mechanism
- A “countercurrent mechanism” simply implies that fluid is flowing in opposite directions right alongside each other (as does highway traffic)
Makes IF hypertonic (1200 mOsm)
- That is, IF has osmolality or high salt content
- Urea from collecting duct adds to high osmolality of IF
Also makes filtrate hypotonic (low osmolality) 100 mOsm
Vasa recta also has a countercurrent flow
- This reduces removal of solutes from interstitium
- Compare to straight-line flow of blood, which would remove all the salt added to the IF by the Henle loop
- This mechanism is called “countercurrent exchange”
| HINT — there are two different “countercurrent mechanisms” | |
|
Countercurrent multiplier mechanism in the Henle loop
Countercurrent exchange mechanism of the vasa recta
|
|
Distal and collecting tubules
Secretion and adjustment of final urine osmolality
ADH (antidiuretic hormone)
- ADH also known as arginine vasopressin (AVP)
- Produced in hypothalamus and released from posterior pituitary gland
- Promotes tubule wall’s H2O permeability
- More water channels (aquaporins) available
- H2O can diffuse out of tubule into hypertonic IF
- Adjusts final osmolality of urine
- You can now have a range of osmolality of urine from 100 mOsm (hypotonic) to 300 mOsm (isotonic) to 1200 mOsm (hypertonic)
- Depends on how much water the body needs to save (conserve) or get rid of to achieve balance (homeostasis)
Aldosterone (hormone from adrenal cortex)
- Increases K+ secretion
- Thus, increases Na+ reabsorption (K+ is “traded” for Na+)
- Makes urea a more dominant solute
- Indirectly increases H2O reabsorption (permitted by ADH)
- Conserves plasma volume
- Renin-angiotensin-aldosterone system (RAAS)
- Renin from the juxtaglomerular (JG) cells, secreted when renal BP is low, promotes formation of angiotensin II
- Angiotensin II promotes release of aldosterone from adrenal cortex
|
ADH and aldosterone are water-conserving hormones. They conserve water in the body by reducing the volume of urine (that is, by retaining water in the body). Click image to enlarge it |
ANH (atrial natriuretic hormone) from atrial walls of heart
- Triggered by increase in blood plasma volume, which stretches the atrial wall beyond normal
- Increases Na+ loss by plasma
- This in turn causes osmosis of H2O out of blood and into the filtrate
- Loss of water from blood tends to lower plasma volume
- ANH opposes the action of aldosterone
- Allows for fine-tuning of water content of body
Urine composition
Water (about 95%)
Ions (mostly sodium and chloride, along with some others including H+)
Urochromes (pigments)
- Mostly bile pigments from breakdown of old RBCs in spleen, etc.
- Could be some beta-carotenes from food / supplements
- Nitrogenous waste
- Urea — waste of breaking down amino acids so they can be used for cellular respiration (in place of glucose)
- Excess drugs, hormones, toxin
Urinalysis — examination of urine to determine composition, including abnormal constituents
|
Review of pH in urinary mechanisms
|
|
H+ is the hydrogen ion (a proton) and is the thing that pH measures. When H+ in a solution goes up, it increases the acidity of the solution—and the pH goes down. When H+ in a solution goes up in a solution, then the solution becomes more alkaline (basic)—and the pH goes up. So if the nephron tubule secretes H+ into the filtrate (out of the blood) then the blood becomes less acid, thus raising the pH of the blood. If the tubule reabsorbs H+ from the filtrate (into the blood) then the pH goes down because we are adding H+ to the blood. Any chemical that reduces H+ in a solution—for example, HCO3– (bicarbonate)—will have the opposite effect as H+. See the Chemistry Learning Outline for a brief review of the concept of pH. FYI, many sources use a color code for acids and bases, based on the classic litmus test:
|
Acid-Base balance
Normal pH range
Changes as small as 0.1 pH unit can have profound effects on cellular functions
- pH 7.34 – 6.80
- Respiratory acidosis (if caused by respiratory mechanism)
- Metabolic acidosis (if caused by anything else)
Alkalosis
- pH 7.46 – 8.00
- Respiratory alkalosis (if caused by respiratory mechanism)
- Metabolic alkalosis (if caused by anything else)
pH-balancing mechanisms
Buffer mechanisms
- In blood plasma
- Several pairs of buffers
- Bicarbonate system
- Phosphate system
- Protein (Hb) system
- Act to neutralize additions of acids or bases
Respiratory mechanism
- Hyperventilation
- Decreases carbon dioxide (Pco2)
- Thus, raises pH
- Hypoventilation
- Increases carbon dioxide (Pco2)
- Thus, lowers pH
Renal mechanisms
- H+ secretion
Compensation
- “Compensated acidosis” and “compensated alkalosis” refer to conditions where the body’s mechanisms for balancing pH are attempting to maintain normal pH despite an abnormal disturbance to the usual pH scenario
This is a Learning Outline page.
Did you notice the EXTRA menu bar at the top of each Learning Outline page with extra helps?
Last updated: October 22, 2019 at 9:10 am