Learning Outline
Respiratory System
A&P 2
Introduction
Meaning
Respiration from re- (“again”) and -spiro- (“breathe”)
Continuous breathing
- Inspiration (breathing in)
- Expiration (breathing out)
Overall function
Gas exchange
- Oxygen (O2) moves into the internal environment (maintaining constantly high concentration)
- Carbon dioxide (CO2) moves out of the internal environment (maintaining constantly low concentration)
Acid-base balance
- CO2 forms carbonic acid in water, thus impacts homeostasis of pH
Fluid balance
- Continual loss of water during expiration impacts homeostasis fluid volume of body
Functional anatomy
Overview of respiratory anatomy
Conducts air under relatively low pressure, thus requiring open (not collapsed) passages
- Each part of passage has structural elements such as cartilage to keep it open
General plan
- Upper respiratory tract is outside the thoracic (chest) cavity
- Lower respiratory tract is within the thoracic cavity
- Gas-exchange (pulmonary) tissues
Respiratory tract is two-way
- Not one-way, like the digestive tract [or bird respiratory tract
]
- Lumen is continuous with the external environment (atmosphere)
Lined mostly with respiratory mucosa
- Covered with moist, sticky mucus
- Ciliated (cilia move the mucus along the tract to keep it clean)
Nose
Nose — nasal cavity
Held open by skull bones and cartilage
Divided into left and right nasal cavities by the nasal septum
- External nares — anterior openings of right and left nasal cavities
- Also called anterior nares, or nostrils
- Singular of nares is “naris”
- Internal nares— posterior openings of right and left nasal cavities
- Also called posterior nares
Lateral walls have three bony shelves (superior, middle, and inferior nasal conchae) that curl downward and inward
- Conchae — “snails” (also called turbinates — “cone-shaped”)
- Conchae divide each nasal cavity into superior, middle, and inferior meatus (tube-like passageways)
- Meatus is both singular and plural (plural can also be meatuses)
- Septum and conchae cause the air to become turbulent, which causes particles to drop out of inspired air rather than being carried further into the tract
Lining
- Respiratory mucosa— pseudostratified ciliated columnar
- Except vestibule is lined with skin (keratinized stratified squamous epithelium)
- Vibrissae — nose hairs
- Olfactory organ
- Roof of L & R nasal cavities
Functions
- Clean inspired air
- Turbulence described above causes particles (dust, pollen, bacteria, etc.) to drop out of air
- Vibrissae (nose hairs) also filter particles, small insects
- Mucus is a sticky film to which particles stick, forming snot —snot is then swept backward and swallowed (the stomach acid and enzymes render contaminants harmless)
- Warm and moisten air
- Air must be warmed and moistened to avoid damage to delicate lung tissues
- Moisture also required to dissolve oxygen so it will diffuse into the blood
- Turbulence increases contact time with moist, vascular mucosa
- Vascularity (high number of blood vessels close to surface) makes mucosa warmer than other tissues
- Air must be warmed and moistened to avoid damage to delicate lung tissues
- Smell (olfaction)
- Conduction of air
- Two-way air movement
- Low-pressure airway
- Phonation
- Phonation is making speech sounds
- Hold your nose shut and see if your words don’t sound different ( then try ordering something at your favorite French restaurant that way—it won’t work)
- Food passageway (in an emergency, or just for fun)
Paranasal sinuses
Hollow spaces in skull connected to nasal cavity via membranous canals
Lined with nasal mucosa
Main purpose is to lighten the skull
Passages are required to allow air pressure inside to equilibrate with atmospheric air pressure
- Also puts sinuses at risk for infection
- If passages swell during infection or allergy (sinusitis), may trap air/mucus inside and create pain
Pharynx
Air passage held open by bone and muscle
- Also a food passage
- Involved in phonation
Lined with respiratory mucosa
- Tonsils provide some immune protection
Three divisions of pharynx
- Nasopharynx — posterior to nasal cavities
- Oropharynx — posterior to oral cavity
- Laryngopharynx — posterior to opening of larynx
Larynx
Larynx — voice box
Held open by 9 pieces of cartilage that form a box with no bottom and hinged lid (epiglottis)
Front cartilages form a neck protrusion called the Adam’s apple
- The passage itself is called the glottis
- The epiglottis (lit. “upon the glottis”) is a the hinged lid that is pushed down to cover the glottis when you swallow
- True vocal folds — lateral folds of elastic fibrous tissue that project toward middle of glottis
- Covered with nonkeratinized stratified squamous epithelium
- Strong vocal ligament along medial edge of fold
- Muscles in/around larynx can pull vocal cords to middle of glottis, shutting down air flow (or reducing air flow, depending on amount of muscle tension)
- False vocal folds — lateral folds of mucosa (ciliated pseudostratified epithelium) just superior to the true vocal folds
- Ventricle — space between true and false vocal folds
- Protection
- Backs up protective function of epiglottis
- Keeps large particles/fluids from passing through the glottis
- Coughing
- Vocal folds shut off glottis completely
- Thorax and abdomen compress, pressurizing air below the larynx
- Vocal folds open suddenly, allowing a blast of air from below to clear out the foreign material
- If the object is lodged in place, it may cause suffocation (see section in book on Heimlich maneuver [abdominal thrusts]
)
- Voice production
- If cords almost cover glottis, passing air causes them to vibrate
- Size of larynx determines base length of cords
- Affected by sex hormones (male larger than female); age (adult larger than child)
- Voice is critical for communication needed for human survival behaviors
- Also makes radio programming possible
- If cords almost cover glottis, passing air causes them to vibrate
Trachea
Trachea — windpipe
Low-pressure air passage to/from thoracic cavity
Held open by C-shaped cartilage rings
- Ciliary escalator (protective function)
- Cilia lining lower respiratory tract and larynx move dirty mucus upward and into esophagus for swallowing, keeping the lower tract free of debris
Flow of cilia.
The “efficient” phase drives mucus forward, then the “inefficient” phase slides back under the mucus without moving it much.
Bronchial tree
Literally, “branched tree” (bronchus — “branch”) (pl. bronchi)
- Primary bronchi branch to each lung
- Secondary (lobar) bronchi diverge from primary bronchi and go to each lobe of a lung
- Tertiary (segmental) bronchi diverge from secondary bronchi and go to each segment of a lobe of a lung
- Successive levels of branching continue, for a total of 23 levels of branching, eventually forming very small bronchioles
Walls of bronchi and larger bronchioles supported by cartilage rings
- Smaller bronchioles have sufficient thickness to stay open without cartilage
Low-pressure airway
- Bronchi and bronchioles have smooth muscle in walls to regulate air flow
- Some gas exchange (in respiratory bronchioles only)
- In-out change of direction of air flow gets less and less further down into bronchial tree, so that by the respiratory bronchioles, there is virtually no tide of in-out flow of air (instead, relatively constant ventilation)
Bronchioles and alveoli
-
AS – Alveolar septum
-
BR – Respiratory bronchiole
-
BT – Terminal bronchiole
-
D – Mucous gland
-
DA – Alveolar duct
-
M – Muscle
-
N – Nerve
-
PA – Branch of pulmonary artery
-
PV – Branch of pulmonary vein
Alveoli
Alveoli (sing. alveolus) — literally “small space”
Microscopic air pouches at ends of bronchial tree
- 300 million total (giving approx. area of 85 m2 = tennis court)
- Blind sacs arranged in a cluster (alveolar sac)
- Interalveolar openings maintain cross-ventilation
Thin wall coated with watery film
- Allows easy diffusion of oxygen (inward) and carbon dioxide (outward)
- Respiratory membrane has three layers
- Alveolar wall (simple squamous epithelium)
- Interstitial connective tissue
- Endothelium of pulmonary capillary
- Respiratory membrane has three layers
- Water tends to “ball up” and cause alveolar walls to stick to one another
- Collapsed alveoli are very difficult to reinflate
- Prevented by surfactant made by Type II alveolar cells
- Surfactant reduces surface tension (attraction between water molecules) and thus reduces likelihood of collapse with normal breathing
- Premature infants often lack surfactant, so they may suffer from respiratory distress syndrome (RDS) as they struggle to re-inflate collapsed lungs with each breath (may be fatal if not treated with mechanical respirator and/or application of surfactant)
- Surfactant reduces surface tension (attraction between water molecules) and thus reduces likelihood of collapse with normal breathing
Contain macrophages that aid in tidying up the place (immunity)
Lungs
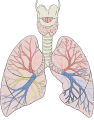
Location: thoracic cavity (left and right pleural cavities)
Size: grow to fill available space
Apex is pointed top; base is broad bottom of each lung
Divisions
Coverings — pleurae
- Visceral pleura (on lung)
- Parietal pleura (lines thoracic cavity)
- Pleural space between layers contains pleural fluid
- Pleural fluid lubricates and keeps lungs “stuck to” inside of thoracic wall (thus holding lungs open)
- Pneumothorax occurs when air gets into pleural space, thus breaking the pleural fluid’s hold (by increasing intrapleural pressure) and causing lung to collapse
Physiology of respiration
Overview of function
External respiration
- Ventilation — keeping fresh air in the alveoli
- Gas exchange — moving air into and out of blood
Transport of gases — in the blood (to / from pulmonary tissues / systemic tissues)
Internal respiration
- Systemic gas exchange
- Cellular respiration— use of oxygen and production of carbon dioxide by cells in order to transfer energy to ATP
Overall regulation of respiration
Ventilation
Primary principle of ventilation
Boyle’s Law — air pressure is inversely proportional to air volume
- Inspiration
- Expand thorax/lungs, increasing the volume
- Decreases alveolar pressure (PA) below atmospheric pressure (PB), causing air to move from atmosphere into lung
- Inspiration: PA < PB
- Mostly the diaphragm that does this
- Compliance
- Ease of stretch
- Allows tissues of lungs/thorax to expand easily during inspiration
- Expiration
- Relax thorax/lungs, decreasing the volume
- Increases alveolar pressure (PA) above atmospheric pressure (PB), causing air to move from lung to atmosphere
- Expiration: PA > PB
- Mostly the elastic recoil of the diaphragm that does this
| Pip — intrapleural pressure (air pressure in intrapleural space) PA — alveolar pressure (air pressure inside the alveoli) PB — atmospheric [barometric] pressure (air pressure of the external environment [atmosphere]) PBJ — peanut butter & jelly |
All P values are mm of Hg
Pulmonary volumes and capacities
- Definitions
- Pulmonary volume — an amount of air moved in or out of the airways
- Pulmonary capacity — a combination of pulmonary volumes
- Spirometry (spiro- “breathe” and -metry “measuring”)
- Measuring pulmonary volumes and capacities
- See table below
- Pulmonary air flow (flow spirometry)
- Total minute volume — volume of air moved per minute (ml/min)
- Forced expiratory volume (FEV) — volume of air expired per second during forced expiration
- Can assess for respiratory obstruction
- Flow-volume loop — graph that shows forced expiration as a loop diagram (thus also showing the peak [expiratory] flow)
- Flow is on the vertical axis of the graph
- Volume is on the horizontal axis of the graph
- Top of the loop is forced expiration; bottom of loop is inspiration
- Measuring pulmonary volumes and capacities
Gas Exchange
Simple diffusion of gases dissolved in water
- Across thin membrane (alveolar wall, basement membrane, capillary wall)
Gas fractions are expressed as partial pressures rather percent by volume
- Dalton’s Law of Partial Pressures
- The total pressure exerted by a mixture of gases (such as air) results from the combined effect of each of the pressures of the individual gases in the mixture
- Thus, the partial pressure of a gas reflects the proportion of that particular gas in the whole mixture
- Partial pressure is expressed as Px where x is the formula for the gas (examples: Po2 or Pco2)
Pulmonary gas exchange — in lungs
- Oxygen (O2) moves into blood
- blood Po2 < alveolar Po2
- Carbon dioxide (CO2) moves out of blood
- blood Pco2 > alveolar Pco2
- Ventilation/perfusion matching
- Perfusion (blood flow) is matched to ventilation (air flow) in each group of alveoli
Systemic gas exchange— in all other tissues
- Oxygen (O2) moves out of blood
- blood Po2 > interstitial fluid (IF) Po2
- Carbon dioxide (CO2) moves into blood
- blood Pco2 < interstitial fluid (IF) Pco
Transport of gases
Oxygen transport
- Small amount (1-2%) of O2 is simply dissolved in plasma
- Most O2 is attached to hemoglobin (Hb), forming oxyhemoglobin (HbO2)
- O2 is attached to the iron (Fe) containing heme groups in the Hb molecule
- Hb loading and unloading of O2 is responsive to local conditions
- Oxyhemoglobin (HbO2) dissociation curve
- O2 is loaded onto Hb when local O2 levels are high —as in the alveolar capillaries
- O2 is unloaded from Hb when local O2 levels are low —as in the systemic capillaries
- More O2 can be unloaded at active tissues than resting tissues
- Conditions that increase O2 unloading from Hb happen to increase as the tissue becomes more active, thus causing additional unloading of O2 in more active tissues
- Conditions that cause further unloading of O2
- Oxyhemoglobin (HbO2) dissociation curve
| The Bohr effect is named for Danish physiologist Christian Bohr (pictured) who first described it in 1904. He is the father of Neils Bohr, the atomic physicist for whom the Bohr model of the atom is named, and grandfather of atomic physicist Aage Bohr —each of whom won a Nobel Prize for his work. |  |
Carbon dioxide transport
- Small amount (about 7%) is dissolved CO2 in the plasma
- Larger amount (about 23%) is carried on the amino acid chains of Hb, forming carbaminohemoglobin (HbCO2)
- Most (70%) of CO2 is carried in the plasma as bicarbonate ions (HCO3–)
|
CO2 + H2O When carbon dioxide (CO2) dissolves in water, some remains dissolved and some forms carbonic acid (H2CO3). The H2CO3 may revert back to CO2 and H2O or it may dissociate into hydrogen ions (H+) and bicarbonate ions (HCO3–). Enzymes in the blood facilitate conversion of CO2 to bicarbonate (and vice versa). CO2 + H2O CO2 + H2O The location of the original CO2 molecule is highlighted in red at each step of the conversion. This chemical equilibrium occurs elsewhere in the body. For example, it it used to make stomach acid and the bicarbonate in pancreatic juice and bile. |
Carbon dioxide handling by the respiratory system affects acid-base balance (pH homeostasis)
- Carbon dioxide in water is carbonic acid, which lowers blood pH
- Blood pH is normally 7.35 – 7.45
- Respiratory acidosis
- Caused by hypoventilation, which decreases the rate at which CO2 is lost by the respiratory process
- “too much” acid (decreased blood pH)
- Respiratory alkalosis
- Caused by hyperventilation, which increases the rate at which CO2 is lost by the respiratory process
- “too little” acid (increased blood pH)
 |
Maintaining normal pH through respiratory mechanisms.
Click on image to enlarge it (and print it out) |
Control of breathing
Many levels of control
- Ordinarily subconscious (regular breathing) but often conscious (speaking, blowing up a balloon, holding your breath, etc.)
Basic respiratory cycle
- Regulated by a network of interconnected regulatory centers in the brainstem
- Still not completely worked out
- Medullary rhythmicity area — in medulla of brainstem
- Ventral respiratory group (VRG) — basic rhythm generator
- Seems to include both inspiratory and expiratory control areas
- Dorsal respiratory group (DRG)
- Signals the VRG to change pattern based on info on Pco2
- Participates in chemoreflexes (chemical reflexes that respond to changes in blood CO2, O2, pH)
- Can be affected by pons (of brainstem)
- Apneustic center
- Regulates length, depth of inspiration
- When damaged — abnormally long, deep inspirations (apneustic breathing)
- Regulates length, depth of inspiration
- Pontine respiratory group (PRG)
- Formerly called pneumotaxic center
- Regulates the apneustic center and medullary rhythmicity area
- Apneustic center
Affected by stretch reflexes in thorax that may help protect you from overinflating your lungs
- Hering-Breuer reflex
Can be overridden by cerebral cortex
- Can be conscious override for speaking, singing, playing an instrument, whistling at your sweetheart, sighing during an A & P exam, and so on
- Can be subconscious override by the limbic system as emotions are expressed
 |
Role of medullary respiration centers in quiet and heavy breathing Click image to enlarge it (and print it out) |
This is a Learning Outline page.
Did you notice the EXTRA menu bar at the top of each Learning Outline page with extra helps?
Last updated: March 28, 2025 at 13:24 pm